Families are encouraged to breast/chest feed exclusively for the first 6 months until complementary foods are introduced. This means nothing besides breastmilk, and medication if necessary. Then you bring your baby to their first pediatrician appointment and they encourage a vitamin D or iron supplement. Why? Doesn’t breastmilk have everything the baby needs? Do you really need vitamins while breastfeeding?
Vitamin D
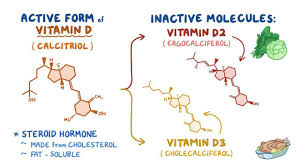
Vitamin D is actually a hormone. It plays a role in bone mineralization, immune function, and calcium absorption. Most of us have been introduced to Vitamin D by way of rickets. Rickets is a bone abnormality caused by extreme Vitamin D deficiency. Rickets was more common decades ago but has made a bit of a comeback, especially with humans who have darker skin or who live in higher altitudes. Much of our Vitamin D comes from the sun, or supplementation. For babies, we depend on breastmilk. It is not recommended to expose your infant to the sun for at least the first 6 months.
Vitamin D In Breastmilk
The problem is breastmilk is often lacking inappropriate levels of Vitamin D. I have often heard individuals express concern that breastmilk doesn’t have Vitamin D at all. This is not true. Breastmilk would have the appropriate amount of Vitamin D available for both the infant and the breast/chest feeding parent IF the breast/chest feeding parent were taking higher levels of Vitamin D in pregnancy or before pregnancy.
What’s Your Vitamin D?
It is not uncommon for someone to be low in Vitamin D. Many of us rely on the sunshine to achieve our daily dose. This can be pretty difficult if you live in a corner of the world where the sun doesn’t shine every day. It has been my experience (maybe yours is different), Vitamin D levels, which can be easily checked by a blood draw, are not checked very often. If I ask for them to be checked, they will. In addition, my levels are always low, even with supplementation. Babies should not start out with a Vitamin D deficiency, as this can impact development. Luckily, you have choices.
Vitamin D Drops
It is recommended babies be supplemented with Vitamin D drops. This can start as soon as you bring your baby home, or once your baby is a few days old. 400 IUs is an appropriate amount and is the amount recommended by the American Academy of Pediatrics. They are pretty simple and easy to administer. Your biggest obstacle with Vitamin D drops will be remembering to give them. Your baby will need this daily, so having a set routine can help.
Supplementing Vitamin D
Another viable option is to supplement yourself with enough Vitamin D for both you and your baby. Luckily, some research is being done in this area. There is some guidance on how to do this. Some families prefer this method, especially if they do not want to give anything additional to their baby. Research also tells us that if a parent supplements with enough Vitamin D for themselves and their baby, they are more likely to continue with appropriate levels overall. If only the baby was supplemented with Vitamin D, the parent continued to be deficient. Basically, breastmilk is lacking in Vitamin D when the parent is deficient. Supplementing only the baby isn’t helping to solve the initial problem.

Researchers looked at Vitamin D levels with lactating parents and their baby. They discovered when the breast/chest feeding parent was supplemented with 6400 IUs daily, this was enough for both parent and baby. This option is enough for the parent levels to stay sufficient.
Iron
What about iron for breast/ chest feeding babies? It is not uncommon to hear medical professionals suggest iron supplements for babies. Is this necessary?
Bioavailable Nutrients
The nutrients in your breastmilk are bioavailable, which means that your baby is able to absorb them better. For example, iron in breastmilk is absorbed into the baby’s system more efficiently than iron from milk-based formulas. Basically, the baby’s body “likes” the iron from the breastmilk much better and hangs on to it for safekeeping. Iron from other sources is foreign to babies’ little system. They kick that stranger to the curb instead of letting it in.
It is true that human milk is low in iron overall. Because it is bioavailable, it is said to be enough to support an exclusively breastfed infant for the first 4-6 months of life. It is recommended to start solids at 6 months, which is when babies can start to receive iron-fortified foods. This will supplement their iron stores. Although the iron concentration is low in human milk, it is thought to be independent of the mother’s iron status and it cannot be increased through maternal diet or iron supplementation (Friel et al).
Delayed Cord Clamping
A study completed with over 400 infants looked at umbilical cord clamping and how this might impact iron stores over time. Delayed cord clamping is when the infant’s umbilical cord is not clamped and cut immediately after delivery. For the first few minutes after birth, there is still circulation from the placenta to the infant. Wait to clamp the umbilical cord for 2–3 min, or until cord pulsations cease. This allows a physiological transfer of placental blood to the infant (the process referred to as “placental transfusion”). The majority of this occurs within 3 min. This placental transfusion provides sufficient iron reserves for the first 6–8 months of life. This can prevent or delay the development of iron deficiency.
Delaying umbilical cord clamping for two to three minutes results in a substantial transfusion of blood from the placenta into the newborn child. Interestingly, one study noted the difference in gender when studying the benefits of delayed cord clamping. Male infants were more likely to have iron deficiency at 4 months than female infants.

Let’s recap all of this information.
Takeaway – Vitamin D
When it comes to Vitamin D, you can either supplement the baby or the parent. Keep in mind human milk is not necessarily deficient in Vitamin D. It is the parent who is deficient. We can supplement the baby, but this will still leave the parent deficient. Since parent and baby come as a package deal, it’s best to make sure both have the correct levels of Vitamin D.
Takeaway – Iron
Iron in human milk is a little different. It is not abundant in human milk. However, what is available for the infant is readily absorbed. Exclusively breastfed babies should have sufficient iron stores until 4-6 months. The practice of delayed cord clamping is a game-changer when it comes to iron for babies. Studies show babies who received delayed cord clamping for at least 60 seconds have better iron stores after 4 months. For more information about vitamin supplements for breastfed babies, you can check out this episode of the Badass Breastfeeding Podcast. As always, if you are ever concerned about the benefits of your human milk, contact a lactation consultant. They will help you figure it all out.
(Friel, J., Qasem, W., & Cai, C. (2018). Iron and the Breastfed Infant. Antioxidants (Basel, Switzerland), 7(4), 54. https://doi.org/10.3390/antiox7040054)





